Importance of Immune Imbalance and Autoimmunity in Nervous System Disorders
VIJENDRA SINGH, PH.D.
Editor: Recent research has been focusing on the role of the immune system in neurological conditions. This important article was posted a few years ago and is being reposted now due to its relevancy. Dr. Singh has been at the forefront of researchers who recognized the role of autoimmunity in autism, obsessive compulsive disorder, PANS, Tourette syndrome, and Alzheimer’s.
Nervous System Disorders as Autoimmune Diseases

 Autoimmunity is a major cause underlying many chronic diseases. There are 85 or so human conditions that are generally considered autoimmune diseases. It is estimated that 55 million Americans suffer from autoimmune diseases, in which the body’s immune system becomes activated abnormally. This number, however, never includes the many more individuals who suffer from nervous system disorders (NSD) and have been found to have autoimmune problems. The exception to this being multiple sclerosis (MS) which is always included as a typical autoimmune disease of the nervous system.
Autoimmunity is a major cause underlying many chronic diseases. There are 85 or so human conditions that are generally considered autoimmune diseases. It is estimated that 55 million Americans suffer from autoimmune diseases, in which the body’s immune system becomes activated abnormally. This number, however, never includes the many more individuals who suffer from nervous system disorders (NSD) and have been found to have autoimmune problems. The exception to this being multiple sclerosis (MS) which is always included as a typical autoimmune disease of the nervous system.
Thus, to start with, I propose that future epidemiological studies must take into account the fact that there is a new patient population which suffers from neurological problems (brain diseases and mental illnesses) and yet shows typical characteristics of an autoimmune disease. Once this population is recognized and accounted for, the number of individuals having autoimmune disease will go up by several fold, not only in the United States but also all over the world.
The credence to this idea stems from several diseases: Alzheimer’s disease affects an estimated five million Americans, and large percentages (65-85%) of those with the sporadic form of Alzheimer’s have autoimmune problems. This group is not represented under the category of autoimmune diseases. Similarly, autism affects three to four million children and adults; up to 85% of them have well characterized autoimmune problems. Many more individuals with Tourette syndrome (TS) and obsessive-compulsive disorder (OCD) have been found to have autoimmunity to the brain. All these populations should be included under the category of autoimmune diseases.
Quite simply put, the financial burden of coping with autoimmune diseases is huge and it will be shown to be much greater once we account for autoimmune diseases of the nervous system that have so far not been tallied in epidemiological studies.
When someone has an autoimmune disease, the immune system goes haywire and begins to attack healthy cells, tissues, and organs. However this occurs in a highly selective way. In the case of brain autoimmunity, the immune system will elicit an autoimmune response against the brain or nerve tissue.
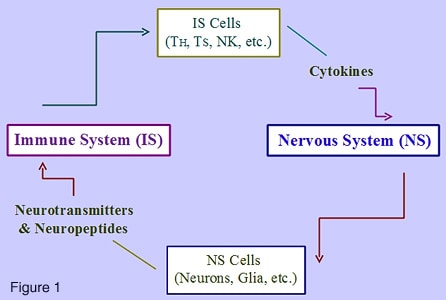
Approximately 25 years ago, we recognized the importance of a reciprocal relationship between our immune system and nervous system, which is illustrated above in Figure 1. As shown, the immune and nervous systems are interconnected and this relationship is mediated by chemical messengers, for example cytokines produced by immune system cells like T helper cells (TH), T suppressor cells (TS), and antigen-presenting cells (APC) – whereas neurotransmitters and neuropeptides are produced by neurons and glial cells. As we know it now, this relationship occurs at both the cellular level as well as the molecular level. But nearly 25 years ago, we postulated (Progress in Drug Research 30:345-363; 1986) that the disruption of this neuro-immune or immune-neural circuitry might actually be the reason behind a wide range of brain diseases and mental illnesses.
Environmental factors such as a viral or bacterial infection, trauma, or brain injury and other factors can easily break down this circuitry. To this end, one of the most important findings in this field is the observation that autoimmune disease of the nervous system is the most common problem that results when the neuro-immune circuitry breaks down. This should prove to be clinically quite relevant because autoimmune diseases of the nervous system could be medically recognized and treated with immune therapies that are currently being used for other autoimmune diseases. This is already beginning to happen as exemplified by immune therapy for individuals with autism, OCD, and TS. Recently, we hypothesized that the disruption of neuro-immune circuitry could cause neuro-immune imbalance in the body, thereby possibly affecting brain plasticity, brainwave pattern, or brain function.
Infections Linked to Nervous System Disorders
What triggers autoimmune diseases is not well known. The common belief is that they are triggered by environmental factors, in particular viruses; for example, Epstein-Barr virus (EBV) and human herpes virus-6 (HHV-6) in multiple sclerosis (MS), measles virus in autism, herpes simplex virus (HSV) in Alzheimer’s disease, and streptococcal infection in OCD and TS. More recent studies have found a closer involvement of EBV in MS (European Congress of Immunology in Berlin, 2009 held in Berlin; Annals of Neurology, 2010; NA DOI: 10.1002/ana.21978). And, when properly tested, just about one in two autistic children has elevated level of antibodies to the measles virus – this is not an exaggeration but a real fact (Annals of Clinical Psychiatry 21:155-168; 2009). Virus infection is now known to change the permeability of the blood-brain barrier, which permits the entry of immune cells and proteins into the brain. Inside the brain, the microglial cells can also produce pro-inflammatory cytokines that are involved in autoimmune process known as neuroinflammation or inflammation of the brain.
Neuro-Immune Circuitry in Nervous System Disorders
 Some 25 years ago, I recognized that our immune system vastly impacts our nervous system (J. Clinical Psychiatry 47:592-595; 1986). This prompted me to study the immune system for two main reasons: First, this might help us discover biomarkers for brain diseases and mental illnesses and secondly, it might help us find novel approaches to therapy with the use of immune modulating agents for these disorders. The fruits of this labor are now beginning to be seen as researchers are now finding these benefits. For example, as summarized in Table 1, like all typical autoimmune diseases, the autoimmunity to the brain has been recognized through laboratory studies of specialized proteins of the immune system (for example, antibodies and cytokines), autoimmunity testing, and immunotherapy. Immune activation, which is the first step in the onset of autoimmunity, has been shown in patients with autism, MS, Alzheimer’s, TS and OCD. Patients with these diseases also harbor elevated levels of autoantibodies that bind specifically to brain proteins: for example, antibodies to caudate nucleus of the basal ganglia (a brain region involved in Parkinson’s disease) in autism, TS, and OCD; antibodies to amyloid protein-beta in Alzheimer’s, and antibodies to myelin basic protein in autism spectrum disorders and MS. Interferon-gamma and interleukin-12, the two proteins of the immune system that initiate autoimmunity, are also activated in patients with brain diseases. Furthermore, many patients also show improvement when administered immunotherapy using intravenous immunoglobulin, plasmapheresis, transfer factor, and other immune modulating agents.
Some 25 years ago, I recognized that our immune system vastly impacts our nervous system (J. Clinical Psychiatry 47:592-595; 1986). This prompted me to study the immune system for two main reasons: First, this might help us discover biomarkers for brain diseases and mental illnesses and secondly, it might help us find novel approaches to therapy with the use of immune modulating agents for these disorders. The fruits of this labor are now beginning to be seen as researchers are now finding these benefits. For example, as summarized in Table 1, like all typical autoimmune diseases, the autoimmunity to the brain has been recognized through laboratory studies of specialized proteins of the immune system (for example, antibodies and cytokines), autoimmunity testing, and immunotherapy. Immune activation, which is the first step in the onset of autoimmunity, has been shown in patients with autism, MS, Alzheimer’s, TS and OCD. Patients with these diseases also harbor elevated levels of autoantibodies that bind specifically to brain proteins: for example, antibodies to caudate nucleus of the basal ganglia (a brain region involved in Parkinson’s disease) in autism, TS, and OCD; antibodies to amyloid protein-beta in Alzheimer’s, and antibodies to myelin basic protein in autism spectrum disorders and MS. Interferon-gamma and interleukin-12, the two proteins of the immune system that initiate autoimmunity, are also activated in patients with brain diseases. Furthermore, many patients also show improvement when administered immunotherapy using intravenous immunoglobulin, plasmapheresis, transfer factor, and other immune modulating agents.
Concerning Tourette syndrome (TS), a recent study has linked the histamine neurotransmitter system with TS and tics. Researchers have identified a rare mutation in the HDC gene complex that encodes 1-histodine decarboxylase enzyme involved in histaminergic neural pathways (NEJM, May 5, 2010 issue). The study suggests that the patients with TS might not be making enough histamine and this reduction in histamine might not be functioning properly on histamine brain receptors. Histamine has different receptors in the brain, for example H2 receptors. It is of considerable interest that H2 receptors are enriched predominantly in corpus striatum or caudate nucleus (Experimental Neurology 66:413-418; 1979), which is also the brain region tissue targeted by an autoimmune response in patients with TS, OCD and autism. Thus it is tempting to speculate that these patients might actually have autoantibodies to brain histamine receptors, much like autoantibodies to brain serotonin receptors in autism (Biological Psychiatry 41:753-755; 1997).
New Findings for Autoimmune Diseases
There are some interesting new findings for autoimmune diseases that may also be relevant to nervous system disorders.
- Autoimmune diseases are associated with oxidative stress (OS) – a sign of reduced function of energy-producing intracellular organelles called mitochondria. Using white blood cells, mainly lymphocytes, the OS has been found in patients with neurodegenerative disorders including Alzheimer’s disease, Parkinson’s disease, schizophrenia and autism. In this regard, a very recent study has shown that OS involves a biochemical defect of a key mitochondrial enzyme called NADP oxidase. Since the OS was found using lymphocytes, this finding may be interpreted as reduced energy level for immune cells, which could ultimately lead to an imbalance of immunoregulatory T cells causing autoimmunity and inflammation.
- Interferon-gamma (IFN-gamma), a pro-inflammatory cytokine produced mainly by T cells, has been shown to increase the expression of immune protein called major histocompatibility complex (MHC) in the brain. IFN-gamma is well known to increase the expression of MHC on neural cells and thereby increase the permeability across the blood-brain barrier. Recently it was found that the enhanced expression of MHC is related to abnormal brain development, which would suggest a role for this protein in disorders like autism and schizophrenia. Since IFN-gamma is a key cytokine inducer of autoimmune response and it is elevated in patients with autism and Alzheimer’s disease, the expression of MHC might also be related to autoimmune pathology of nervous system disorders.
- Vitamin D has recently been found to play a crucial role in activating immune response defenses. It controls human T cell function to elicit an effective immune response against invading viruses and bacteria. It was found that without sufficient intake of the vitamin, the killer cells of the immune system — T cells — will not be able to react to and fight off serious infections in the body. (Nature Immunology, 2010; DOI: 10.1038/ni.1851). Thus the insufficient amounts of vitamin D causes an imbalance of immunoregulatory T cells. Since these cells are abnormal in autoimmune diseases, vitamin D will play a vital role in nervous system disorders. Indeed, many patients with nervous system disorders are deficient in vitamin D and therefore a daily intake of this vitamin is highly recommended.
- Poor sleep or sleep deprivation increases inflammation as shown by elevated levels of CRP. This serum protein is an acute-phase protein and is associated with autoimmune disease. This finding is relevant to nervous system disorders. For example, children with autism generally are sleep deprived and do not have good sleep patterns, and elevated levels of CRP have been found in children with autism (Annals of Clinical Psychiatry 21:155-168; 2009).
- There is reason to believe that stem cell therapy can be used to help patients with autoimmune diseases, including nervous system disorders. Stem cells, in particular those of the bone marrow, are committed to become immune cells like lymphocytes. IFN-gamma is a front-line immune defender against microbial infections. It also regulates normal development of immune cells from bone marrow-derived stem cells; the process is known as hematopoiesis. A recent study has found that IFN-gamma prompts and promotes the production of immune cells from bone marrow progenitor stem cells during a bacterial infection (May-June 2010 issue of Nature). Because IFN-gamma is a pro-inflammatory cytokine, this finding has tremendous potential for immune therapy with stem cells for nervous system disorders. This would be a novel mechanism for stem cells to produce normal functioning immune cells that in theory should help overcome immune imbalance and therefore autoimmunity. An alternative approach would be to use growth factors and other nutraceuticals to provide an environment that will be conducive to yielding immune cells, neural cells, or other type of cells. Among various factors, vitamin C is being used to cultivate and harvest neural cells in tissue culture systems of the stem cells. When people think of stem cell therapy for neurological diseases they generally only think of repairing nerve cells in the brain. But there should be more emphasis on reconstituting immune cells since the immune cells vastly impact nervous system function. Ideally, the attempts should be directed toward rebuilding both the nerve cells as well as the immune cells from stem cells.
Future Remarks for Nervous System Disorders
To conclude, several lines of scientific evidence suggest a pathogenic role of brain autoimmunity in nervous system disorders (NSD). This patient population must be accounted for in all future epidemiological studies if we are going to realize the actual impact of autoimmune diseases. Immunotherapy with immune modulating agents offers a novel promising approach to helping those affected with these medical conditions. Autoimmunity in the brain may also cause a shift in brain waves or states thereby resulting in a functionally “imbalanced brain.” This type of autoimmune injury to the brain would in fact be very similar to traumatic brain injury (TBI) and the outcome may be long lasting because autoantibodies will bind to brain proteins and impair brain function. Thus, I would like to suggest that we should administer immune therapy first to bring about “Immune Balance” before administering medical or alternative treatment for nervous system disorders. It is furthermore implied that the immune balance means establishing a normal balance of immunoregulatory function of T cells (balance between T helper and T suppressor cells), unlike simply boosting or suppressing the immune function. This approach might be particularly suitable and effective in patients who receive neurotherapies and neurofeedback technology to balance the brain function. Naturally, therefore, the immune balance would be a pre-requisite.
According to the World Health Organization (WHO), the financial burden of all brain diseases and mental illnesses surpasses that of cancer and heart disease. Since up to 85% of patients with nervous system disorders have scientific evidence of autoimmunity, a huge proportion of this population could potentially be helped by immune balancing modalities to target autoimmunity in the brain. The first step is to recognize that a vast majority of nervous system disorders involving autoimmunity are autoimmune diseases similar to all other medically-recognizable autoimmune diseases. Then, focusing on immune balance first, before the neurotherapy, might very well prove to be a novel approach to helping patients suffering from nervous system disorders.