2019 Guidelines for Treating Tourette’s and Tics: A Failure and a Farce

Editor and Director, Sheila Rogers DeMare
After several years, a new set of medical guidelines for treating Tourette’s and chronic tic disorders was released. It fails miserably in meeting the needs of patients.
The document, published in the leading medical journal Neurology, does little to move the prevention and treatment of these disorders forward.
New treatment areas of promise are blatantly ignored in the 2019 guidelines, and the development of useful new directions is stalled.
To date, conventional medicine has not offered patients and families an explanation of why tics occur, or how to reduce them without strong drugs or complex behavioral training. (Or, when all standard approaches fail, implanting electrodes in the brain.) I had hoped that new guidelines would open new avenues. But it is just more of the same.
“Tourette syndrome is a genetic problem and there is no cure,” is the standard line. Chronic tics? Well, the docs tell us they might go away on their own. Or then again. . . they might not. If symptoms get a lot worse there’s always medications that most people want to avoid due to side effects.
Patients and families leave doctors’ offices with few answers.
Based on the 2019 guidelines, we should not expect that approach to change any time soon, and that is the key failure of this new effort.
A summary of the new guidelines
 These guidelines were published in the May 2019 issue of the popular medical journal Neurology and published online (as of this writing): See here.
These guidelines were published in the May 2019 issue of the popular medical journal Neurology and published online (as of this writing): See here.
According to report, the American Academy of Neurology, convened a group of nine physicians, two psychologists, and two “patient representatives” to develop new practice recommendations for treating chronic tics and Tourette syndrome. The committee is responsible for advising on approaches that will affect millions of people worldwide.
Forty-six recommendations were made by this group on how to assess and manage Tourette’s and chronic tics.
I was eager to see the advice and then very disappointed to realize it was largely the same old protocols as before.
Grouped together the 46 suggestions include:
- Counseling recommendations on the natural history of tic disorders;
- Psycho-education for teachers and peers;
- Assessment for psychiatric comorbid disorders (in other words, does a patient have a condition like attention deficit hyperactivity disorder [ADHD] or obsesssive-compulsive disorder [OCD] along with the tics;
- Periodic reassessment of the need for ongoing therapy;
Treatment options are
- “Watchful waiting”
- Behavioral therapies (i.e., CBIT)
- Medications;
- Deep brain stimulation
What’s missing: Doctors will be seeking guidance from this Neurology article to learn how to handle cases of Tourette’s and chronic tics in their offices. Yet, there is no advice on how to explore what may actually be causing the tics.
and chronic tics in their offices. Yet, there is no advice on how to explore what may actually be causing the tics.
If someone has a recurring stomachache, it is assumed a physician will try to figure out why. If the patient has a pain in the chest, there is the same goal, to determine a cause. If someone has breathing problems, a clinician strives to find out why. But if a patient has tics? No effort is made to understand why–because doctors follow guidelines that do not include that step.
Readers who are unfamiliar with how tic disorders are typically viewed by physicians might be surprised to learn that the health status of the patient is rarely considered when treating tics. Nor is the person’s prior or current environment, diet, or lifestyle considered during an office visit, a common medical practice.
Instead, a simple checklist is used to decide what category of tics might be present so a diagnostic label can be given. Goal accomplished! But while a label may satisfy the doctor and the insurance company, it does not satisfy the patient.
 People are looking for real answers. They want to know why they have the tics and what they can do to reduce them. And, they want to know specifically why tics flare at some times and subside at others.
People are looking for real answers. They want to know why they have the tics and what they can do to reduce them. And, they want to know specifically why tics flare at some times and subside at others.
Our organization, Association for Comprehensive NeuroTherapy (ACN), has collected information on these conditions for more than 25 years.
We have learned that doctors and patients who have successfully reduced or eliminated symptoms of Tourette’s and other tic disorders have often done so by exploring the issues below and addressing them when needed. (We offer a comprehensive overview of Tourette syndrome here.)
A partial list of issues that can impact the nervous system and are ignored in the 2019 Guidelines
- Environmental factors
- Viral, bacterial, fungal, parasitic, and other infections
- Allergies: Pollens, mold, ragweed, insect, dust mite, foods and more
- Food intolerance and sensitivity beyond classic allergy; reaction to food additives
- Nutritional and mineral imbalances
- Toxic chemical exposures and overloads
None of the recommendations in the 2019 guidelines consider possible causes of tics. These factors above have been reported by doctors and the tic community for decades!
Repeated calls for research in these areas go unheeded, while the medical community is only familiar with the status quo. And patients suffer.
Doctors and patients need to be educated on triggers for tics
There have been thousands of reports of people experiencing one or more “triggers” for tic symptoms. The first report came more than 40 years ago. (Read a physician’s report of his daughter’s triggers in this article from the early 1980s)
Our organization has found through survey responses and case reports that triggers fall into eight main categories. When personal triggers are identified and avoided, symptoms are often reduced or eliminated completely.
Types of triggers as categorized by ACN/Latitudes.org:
- Sensory influences
- Allergens
- Food/Drink
- Toxins
- Medications
- Lifestyle
- Physical imbalances
- Weather
For more information on tic triggers see Stop Your Tics by Learning What Triggers Them.
The missed opportunity: The role of the environment
The 2019 guidelines could have encouraged physicians to explore lifestyle, environmental issues, allergens, gastrointestinal, immune, and dietary factors–consulting with others outside their field as needed.  They could have promoted a more comprehensive approach to dealing with Tourette syndrome and chronic tics, one that would lead to new answers and actually help heal people.
They could have promoted a more comprehensive approach to dealing with Tourette syndrome and chronic tics, one that would lead to new answers and actually help heal people.
They could have suggested that when neurologists can’t help a patient they should refer out to practitioners in other fields who can explore medical issues that may be playing a role.
But rather than expand the understanding of what causes these conditions, they simply call for more of the same types of focus:
1) talk-therapy;
2) different types of drugs;
3) behavior therapies, and
4) deep brain stimulation (electrodes implanted in the brain).
The 2019 guidelines disappoint in their utter failure to encourage clinicians to look for the cause of tic symptoms–a basic principle of medicine. They should have offered new insights but do not.
 The new guidelines are harmful and a farce
The new guidelines are harmful and a farce
When compared to the current conventional approach to tics—which is widely acknowledged in surveys of the tic community as unsatisfactory—little of substance has changed with the new recommendations.
How do the 2019 guidelines differ from the previous set? The changes are summarized here.
- In the past, patients dealing with tics that were not considered life-altering were told by doctors to simply go home and see if symptoms improved on their own. That advice will now be referred to as “watchful waiting.”
- Behavioral therapies, which aim to train patients to alter the way their tics are expressed, is now suggested as the first line of treatment.
- Additional attention is placed on counseling and outreach education.
- Emphasis is given to discussing the harm that medications can cause while weighing possible benefits.
Here’s why these guidelines are inadequate and harmful
- Clinicians assessing tics will continue to rely on simplistic checklists rather than medical evaluations
 The guidelines fail to encourage practitioners to assess possible factors that could be contributing the the tics. This could require consultation with experts in other medical fields.
The guidelines fail to encourage practitioners to assess possible factors that could be contributing the the tics. This could require consultation with experts in other medical fields. - The team lacks knowledge and experience in key areas This document was developed by a team that is apparently ignorant of the potential role of diet, nutritional and metabolic status, allergens, toxins, the gut-brain connection, infections, and the immune system in nervous system functioning. As such, they have ignored these critical areas that have proven important in many health conditions and hold promise for the understanding and treatment of Tourette syndrome and other tic disorders.
- Mention of symptom triggers is completely lacking Symptom triggers are not a new concept and have been widely reported for tics for decades. A few possible triggers in migraine, for example, are fragrances, flashing lights, aged cheese, and MSG (monosodium glutamate), among many others. Similar patient-specific triggers exist for Tourette’s and tics but are never discussed by leading advocate groups nor these guidelines. The Neurology article does not even use the “triggers.” This team appears content to leave patients and families in the dark on possible ways to improve health and reduce suffering through the identification and elimination of tic triggers.
Tics are not considered in a holistic manner in these new guidelines. Rather, they are apparently viewed as an independent, mysterious phenomenon–much as medicine looked at health issues 100 years ago. This document reinforces that antiquated approach.
In a nutshell: This one sentence tells the sad story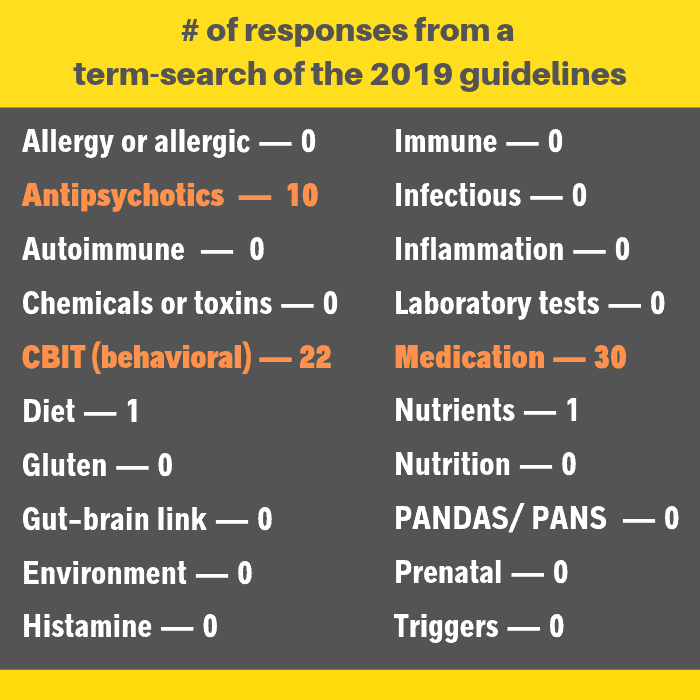
The 2019 guidelines contain more than 5,200 words. Only one sentence focuses on future directions that could truly be helpful in providing safer and better approaches to tics.
That sentence is: “Future research on the effect of special diets, nutritional supplements, and exercise on tic severity is needed.” This is the closing statement to the whole report, as if an obligatory afterthought.
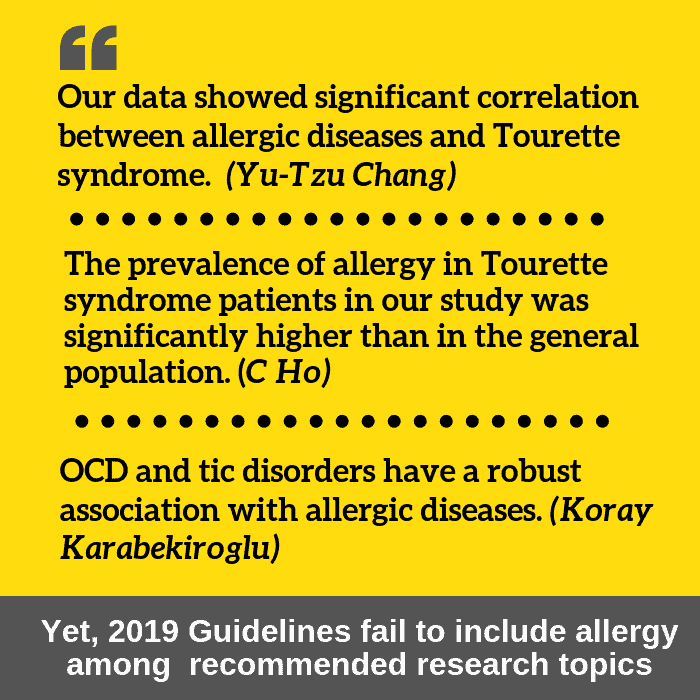
And those words omit recommending the study of the role of the immune system, infection, allergy, toxins, and the environment in tics–a blatant oversight. Each of these areas has been linked to tics in published journal research.
In fact, the entire role of the environment in Tourette’s is ignored, even though it is widely recognized as playing an important role in this condition. This disqualifies this document as being unbiased and relevant.
What, then, does this advisory team consider the most important focus for future research?
Unfortunately, more of the same! Behavioral therapies; plenty of medications: first-generation antipsychotic fluphenazine; selective D1 antagonist ecopipam; dopamine depleters, tetrabenazine, deutetrabenazine, and valbenazine, cannabis and Chinese medicines; deep brain stimulation. Relatively new to the table is cannabis and Chinese medicine.
What is urgently needed for progress? A more inclusive expert multidisciplinary team
A collaborative team of practitioners that includes international leaders from fields of allergy, immune function, laboratory testing, nutrition, chemical sensitivity, and environmental medicine (among others) needs to be consulted when developing the best approaches to chronic tics and Tourette’s.
The very brightest and best should be sought out to change the currently stunted direction of research on tics. New, fresh protocols are desperately needed.
Of course, this would mean that mainstream psychiatrists, psychologists, behavioral therapists, and related practitioners would have to admit that finding answers for tics and Tourette’s requires more than their limited area of practice can offer.
Until the required change in leadership takes place, ACN Latitudes.org will continue to provide the tic community and practitioners with innovations in treating these conditions through our books and this website.
Research Articles on Tourette Syndrome
Click for a sampling of research on Tourette syndrome that is overlooked in these guidelines
Sheila Rogers DeMare






Sheila, I’ve been following what you do for years. This is unbelievable–same ol’ same ol’. Don’t get frustrated, you are still reaching people. You have to wonder how much these leaders really care. No surprise that doctors don’t know how to help our kids. :(
Thank you for the support BGM. Truth is I do get very frustrated at how factions of the medical community cling to their approaches to Tourettes and tic disorders when those efforts clearly are not good enough. I don’t know how their conscience allows them to ignore positive reports from other disciplines. And, as you say, doctors don’t know any better because they take their lead from guidelines like this.
Not sure I am following. Are you saying that traditional medical treatment is NOT addressing the issue of tics? That they are only wanting to throw more medication at the problem rather than looking for the underlying reasons for the syndrome?
Are you also saying that there could be other key inflammatory reasons for the inflammatory cells (TH17 cells) to sit in the areas of the brain that cause this behavior?
Could they have entered and crossed the blood brain barrier (BBB) through the olfactory bulb as the result of an infection? maybe strep? Could this possibly be related to the inflammatory auto immune response?
What the hell does it take for the medical community to stop looking to the pharmaceutical industry for all their answers? Research is showing us how all this is occurring and why won’t they listen?
Treat the underlying infection causing the brain inflammation.
Teresa, your sarcasm beautifully expresses your frustration. I remember seeing a book Brain Allergies 20+ years ago (updated version) that outlined factors–infections, food, and chemicals– that could create inflammation in the brain, resulting in a number of neurological reactions. Dr. Philpott was on our advisory board and unfortunately passed away in 2009. At the time of the first edition, his book was very forward-thinking. Today the potential damage from inflammation is widely recognized, making it all the more shocking that neurologists often turn a blind idea to the issue and simply, as you say, throw drugs at disorders without exploring inflammation as an underlying cause.
I don’t understand how they can get away with this for so many years. We saw tics get worse with an infection and I know lots of other people have too. That isn’t even on their radar? Something is very wrong.
I couldn’t agree more….what about the role of an infection affecting the immune system and causing inflammation in the brain. Tics are a symptom seen in PANDAS. It also causes Tourette’s like symptoms. And certainly tics are seen with Lyme’s disease…another infection. But again, not on their “list”….
Rosalyn after reading your note I added “inflammation” to the list in the article graphic. First I searched for it in the guidelines, nothing came up– no surprise. Inflammation is one of the hottest topics in medicine right now, but apparently dismissed out of hand by the group that developed the guidelines. Lyme and tics for sure, thanks for pointing that out. . . conventional practitioners usually don’t make the connection.
My stepson has Tourettes, age 11. The pediatrician referred us to a neurologist and to be honest that was no help. I didnt want to use a blood pressure medication for him. At the time the vocal tics were minor compared to the muscle tics. This was a few years ago and we came across your Natural Treatments book. It gave us hope and opened our eyes to so many new ways to approach things. He’s doing really good now and our whole family is healthier now that we changed our eating habits and went natural. Thank you for what you do.
I may not have all the answers but I know beyond doubt that my relative developed tics after getting a flu shot. That’s exactly what caused it.
Sharon, I hope your relative’s tics have resolved? That reaction is totally believable. We have an article on this documented in research here.
Here’s a separate PubMed research article.
This is what the CDC says about the flu vaccine and thimerosal. Note that individual single-dose vials can be (and we say should be) requested . Even though most vaccines in the West do not contain mercury any more, someone could be hypersensitive to it–in addition to a negative reaction to other ingredients.
Wow. How am I going to go to sleep tonight? Your article got me so worked up. Thanks for summarizing the guidelines from Neurology. I want to say I’m shocked, but somehow, I’m almost numb from more of the same… why can’t the mainstream medical community get behind what ACN has been advocating for decades now? Thanks for sticking with what you’ve been so passionate about all these years, Sheila. One day, I hope the medical community will look back on these days, shaking their heads in disbelief that it took them so long to start looking into triggers for tics. Hope for everyone’s sake that day comes soon!
Candice, hearing your message helps me keep my sanity about this. It is so unbelievable that commonsense approaches are ignored by leading organizations in this field–quite intentionally, I believe. Someone recently pointed out to me that major change in both society and in medicine can take 40 or 50 years. It’s been over 40 years for this field and I barely see the needle moving, which is why I have to keep advocating. Somehow I keep hoping that with all the access to online information that new concepts would be shared and investigated more readily–but apparently not so!
This is so disappointing. I find it unconscionable that nothing has changed since my brother was diagnosed in 1965. Sadly, these guidelines are gospel to most physicians. Just last week, I met with the medical director of a laboratory who was furious that doctors didn’t understand how to interpret results for syphilis testing. Someone new to the industry asked why. “Because they are educated on laboratory diagnostics for one day of their entire four years in medical school,” I replied. Physicians cannot learn everything, and they are too busy to keep up with new advances. As a result, they depend on published guidelines.
Here’s the rub: When it comes to obesity, heart disease, and impaired cognitive function; the medical community has no problem looking to the epidemiology of diet, environment, and the potential exposure to toxic substances. Why then is it so hard to accept that the same could be true for Tourettes?
Michael, you hit the nail on the head. A doctor who recently began his practice (and had the #1 score in the state on board medical exam) read my book on tic triggers and environmental medicine and said, “We were never taught anything about this in med school.” You are right, Michael. They depend on guidelines like this that sadly failed to move the treatment options forward.